SAN DIEGO, CA — In 2019, Jim Bartell sat beside his dying son Ryan in a Washington state hospice facility, powerless against his suffering. Ryan was terminally ill with pancreatic cancer, his final days marked by intense pain, nausea, and opioid-induced comatose days. But after relocating him to a facility that allowed medical cannabis under physician supervision, Ryan’s final days were characterized by a higher quality of life as he was alert, pain-managed, and able to say goodbye to his loved ones.

That experience led Jim Bartell to co-author California Senate Bill 311, also known as Ryan’s Law, which was signed into law in California in 2021. It permits terminally ill patients in health care facilities to use medical cannabis in non-smokable form for palliative and hospice care.
Today, a growing national movement is pushing to make that right a reality in the states where medical cannabis is currently legal.
“No one should have to suffer in their final days when a safe, effective option exists,” says Bartell, now the founder of the Ryan’s Law Foundation. “This is a matter of dignity, compassion, and choice.”
What Is Ryan’s Law?
Ryan’s Law, or CA SB 311, ensures that patients in California with a terminal illness (defined as a prognosis of one year or less to live) can access and use medical cannabis on-site at healthcare facilities, provided they comply with state cannabis laws. The law prohibits smokable and vape forms, but allows tinctures, capsules, edibles, and oils.
The California Department of Public Health issued a guidance letter in early 2023 encouraging facilities to adopt Ryan’s Law and informing them of compliance.
Since its passage, the law has opened the door to similar legislation in other states, notably Oregon’s HB3214 and Rhode Island’s H5630, both modeled after California’s framework; and derivative models passed into law Maryland in 2024 and North Dakota in 2023.
Why This Story Matters
More than 1.7 million Americans receive hospice care every year, according to the National Hospice and Palliative Care Organization. Many of them endure unrelieved pain, anxiety, insomnia, and loss of appetite. While opioids remain standard, they often leave patients sedated, disoriented, or dependent.
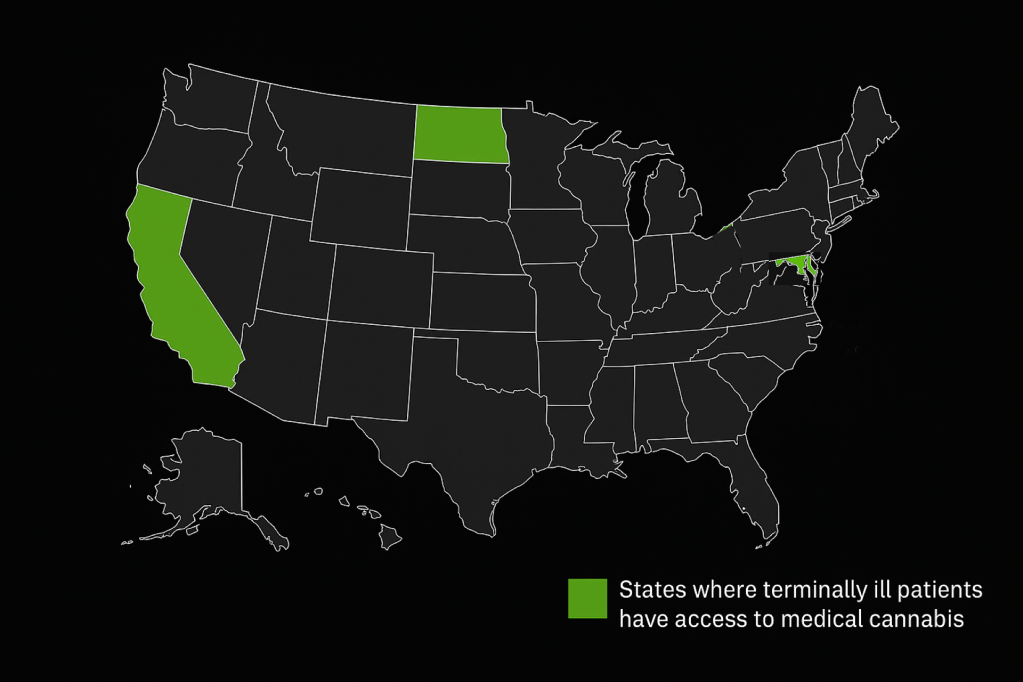
At the same time, 38 states and the District of Columbia have legalized medical cannabis, yet only 3, California, Maryland, and North Dakota, explicitly protect its use in end-of-life care facilities.
This legal gray area leaves families like the Bartells to make desperate, last-minute decisions during such a vulnerable time. And it leaves patients with terminal diagnoses at the mercy of inconsistent state laws, facility policies, and the stigma still attached to the plant.
The Legal Gap and the Fight to Fix It
“We’ve been in rooms where a patient is crying for help, and the nurse says, ‘I’m sorry, we can’t allow that here,’” says Heather Manus, an RN and longtime cannabis nurse advocate who helped draft language for Ryan’s Law.
Manus, founder of the Cannabis Nurses Network, has worked closely with hospice and palliative care teams. She emphasizes that cannabis not only eases pain but also restores quality of life in ways other medicines can’t.
“It gives patients back their voice, their clarity, their appetite. It’s a bridge back to humanity in their last days” added Manus.
But barriers remain.
Despite medical cannabis being legal in dozens of states, federal prohibition still casts a long shadow. Facilities that receive federal funding, like hospitals, VA centers, or nursing homes, are at risk of violating DEA regulations or experiencing denial of federal reimbursements by allowing cannabis on site.
Even in California, implementation has been spotty.
“As written, the law prohibits health care professionals from administering cannabis medicine to patients, so patients with dementia or other conditions (such as end of life) that make them unable to self administer, have no access,” added Megan Mbengue, MS-MCT, BSN, RN and founder of EntheaCare.
“There’s no enforcement mechanism in the law,” says Sandra Guynes, MSN, RN, OCN in San Diego, and founder of the advocacy organization Cannabis Nurses of Color. “Facilities can still say no. And most staff can’t touch the product or help the patient dose and that puts the burden back on families.”

During a San Diego Women of Color in Cannabis event, Guynes expressed her support for the intention behind Ryan’s Law but sees it as “a major challenge without explicitly requiring support from medical staff for the patient.”
The Science & Safety Behind Cannabis at End-of-Life
Research into cannabis for palliative care is growing. Nurses and physicians alike report improved outcomes when patients are allowed to use it.

In a 2023 study published in Oncology Nursing News, hospital staff in an inpatient cancer unit reported “positive patient experiences” after introducing medical cannabis into their pain. Patients became more communicative, required fewer opioids, and expressed higher satisfaction with their care.
“The evidence is already there,” says Guynes. “What’s missing is policy. Uniform policy that supports providers, protects patients, and standardizes care.”
The Highs and Lows
Efforts to expand Ryan’s Law nationwide have faced mixed outcomes. Oregon’s HB 3214 and Rhode Island’s H5630, both introduced early this year with the intent to mirror California’s law, ultimately did not pass. Despite early optimism and support, these bills stalled in the legislative process, highlighting the persistent challenges of advancing cannabis-related policy, even in progressive states.
Still, momentum continues in New York with the introduction of Assembly Bill 2025 A8469, and in Pennsylvania with Senate Bill 1035. If passed both bills would allow terminally ill patients to use medical cannabis in hospitals and nursing homes. Jim Bartell, medical professionals, Americans for Safe Access, and the Ryan’s Law Foundation serve as advocates standing by the respective state representatives sponsoring the bills (Assemblymember Amy Paulin (D-Scarsdale) in NY, and Senator John Kane (D-District 9) in PA.
“Even when bills don’t pass, they spark the conversations we need to have. The Ryan’s Law Foundation will continue its mission to fight for compassionate care implementation in hospice care for terminally ill patients in all states where medical cannabis is legal.” says Jim Bartell. “We are in the process of drafting legislation for New York, Virginia, and Hawaii.”
“This isn’t about promoting cannabis,” says Ben Hueso, former California Senator, co-author of Ryan’s Law CA SB311. “It’s about expanding access to compassionate care.”
Hueso and Bartell have partnered with national organizations like Americans for Safe Access and NORML to lobby for expansion into other states.
The Ryan’s Law Foundation Goes National

Established in 2023, the Ryan’s Law Foundation has begun outreach campaigns in New York, Virginia, Michigan, Colorado and Hawaii; all states with medical cannabis programs but no policies for in-facility use.
The foundation also trains providers, educates lawmakers, and helps families understand their rights.
“Our goal is to make Ryan’s Law the model for all 50 states,” says Bartell. “We’re not done until every terminally ill American has the option to spend their last days on their own terms, with dignity, relief, and choice.”
Voices from the Frontlines: Patients and Families
John Kazanjian, a medical cannabis patient who lost his life-partner to liver cancer in 2017, credits cannabis for helping his partner remain conscious and pain free during his final days. That experience inspired him to advocate for cannabis and to volunteer with hospice patients in Southern California.

“It’s not about getting high,” Kazanjian says. “It’s about being present. I’ve seen patients use CBD drops or a low-dose edible and be able to eat, talk, smile again. That’s a gift.”
In many cases, families don’t even realize cannabis is an option until it’s too late. That’s where Ryan’s Law, and those advocating for it, are trying to change the system.
What’s Next: A Call for Federal Guidance

Advocates are now calling for a federal framework that protects state-authorized cannabis use in end-of-life care. “A federal carve-out, or guidance from HHS or CMS, could reassure facilities that allowing cannabis won’t put them at legal risk” Ken Sobel, an attorney in San Diego, focused on cannabis law.
Until then, Bartell and allies continue pushing one state at a time.
“We’ll win this fight with human experiences,” says Sobel. “With families sharing what happened to their loved ones. With nurses, doctors, and lawmakers standing together.”
Death with Dignity Is a Human Right
Cannabis at end-of-life is no longer a fringe idea. It’s a growing demand, backed by science, personal stories, and legal precedent. But until Ryan’s Law becomes the standard, not the exception, millions of dying Americans will face their final days in opioid fog.
In a country that prides itself on freedom and choice, that’s a contradiction worth fixing.
“We can’t bring Ryan back,” says Bartell. “But we can make sure no one else suffers the way he did. That’s our mission. That’s Ryan’s legacy.”
To extend the reach and engagement of this reporting, a dedicated Instagram page has been launched to document the national journey of Ryan’s Law. The platform invites the public to follow, share, and take part in the conversation around compassionate end-of-life care. Follow and share @RyansLaw_Progress!
Click the button to experience Ryan’s Law Interactive Timeline: Follow key moments, advocacy milestones, and the growing national movement to protect the rights of terminally ill patients. ⬇︎
Leave a comment